Cohort study of the effect of surgical repair of symptomatic diastasis recti abdominis on abdominal trunk function andquality of life
A. Olsson1,3 , O. Kiwanuka1,3, S. Wilhelmsson4, G. Sandblom1,3 and O. Stackelberg1,2,3
1Department of Clinical Science and Education, Karolinska Institutet, Södersjukhuset, and 2Unit of Cardiovascular and Nutritional Epidemiology Institute of Environmental Medicine, Karolinska Institutet, 3Department of Surgery, Södersjukhuset, and 4Functional Area Occupational Therapy and Physiotherapy, Allied Health Professionals Function, Karolinska University Hospital, Stockholm, Sweden
Correspondence to: Dr A. Olsson, Department of Clinical Science and Education and Department of Surgery, Södersjukhuset, Sjukhusbacken 10, 118 83 Stockholm, Sweden (e-mail: [email protected])
Background: During pregnancy, women are at risk of developing persistent symptomatic diastasis recti abdominis (DRA), which may have a detrimental effect on their physical function and quality of life (QoL). The aim of this prospective cohort study was to determine the effect of surgical repair of DRA on abdominal trunk function, urinary incontinence and QoL in postpartum women with trunk instability symptoms resistant to training.
Methods: Postpartum women with diagnosed DRA and training-resistant symptoms underwent double-row plication of the linea alba. Abdominal trunk function was evaluated as the primary endpoint using a multimodal examination tool, the Abdominal Trunk Function Protocol. Recurrence was assessed by CT, urinary incontinence was evaluated using the Urogenital Distress Inventory (UDI-6) and Incontinence Impact Questionnaire (IIQ-7), and QoL was assessed with the Short Form 36 (SF-36®) questionnaire. All subjects were examined before and 1 year after surgery.
Results: Sixty women were recruited. There was no DRA recurrence at the 1-year follow-up. Self-reported abdominal trunk function had improved in 98 per cent of patients, with a mean score improvement of 79⋅1 per cent. In the physiological tests monitored by a physiotherapist, 76 per cent performed better and endured exercise tests longer than before surgery. All SF-36® subscales improved significantly compared with preoperative scores and reached levels similar to, or higher than, the normative Swedish female population. For the UDI-6 and IIQ-7, 47 and 37 per cent respectively reported fewer symptoms at follow-up than before surgery, and 13 and 8 per cent respectively reported more symptoms.
Conclusion: In this series of postpartum women presenting with DRA and symptoms of trunk instability resistant to training, surgical reconstruction resulted in a significant improvement in abdominal trunk function, urinary incontinence and QoL.
Funding information
Stockholm County Council
Swedish Society of Medicine
Paper accepted 26 June 2019
Published online 11 September 2019 in Wiley Online Library (www.bjsopen.com). DOI: 10.1002/bjs5.50213
Introduction
Diastasis recti abdominis (DRA) is a common and expected condition during pregnancy1, owing to mechanical stretching, expansion and hormonal changes2. The condition is often characterized by bulging or sagging in the abdominal midline during abdominal muscle contraction. Although no consensus regarding the definition of DRA exists, it is often defined in the literature as separation of the recti greater than 22–30 mm3–5. DRA usually regresses to its prepregnancy width, but the condition persists in 32–46 per cent of postpartum women6–9. Reported risk factors for persistent DRA include maternal age, multiparity, caesarean section, macrosomia and multiple gestations10. A persistent DRA may be associated with abdominal trunk instability, which could result in development of lower back pain, lack of trunk strength and urinary incontinence11–13. However, it remains unclear whether the DRA actually causes these symptoms or not. Although inconclusive7,8,14, persistent lower back pain after pregnancy has been reported in 11–21 per cent of postpartum women15–17.
The management of DRA is also a subject of discussion. Conservative management with training and weight loss is generally advised as first-line treatment. There is no strong evidence that training during pregnancy and in the postpartum period decreases the risk of persistent DRA18 –20, although some studies8,21 have reported that specific exercises could increase abdominal trunk stability and reduce some of the associated symptoms. Surgical reconstruction has been reported to restore abdominal trunk function22–26 and improve lower back pain and urinary incontinence24,26. General awareness of symptomatic DRA is poor, and patients are commonly advised to undertake non-specific physical training, or told that the condition is only cosmetic in nature. To evaluate potential treatments for persistent symptomatic DRA, a standardized and comprehensive multimodal protocol, able to capture the wide panorama of dysfunctions associated with the condition, is required. Thus, symptomatic persistent DRA lacks clarity of definition and management18,20. This study aimed to evaluate the effect of surgical reconstruction of DRA in postpartum women, where no improvement in symptoms had been achieved by adequate physical training, using a standardized multimodal examination.
Methods
Women with symptomatic DRA were recruited between January 2015 and March 2017. All first underwent ultrasound measurement of the DRA, CT to localize any concomitant ventral hernia, and assessment of trunk function by a physiotherapist. Potential candidates received an individualized trunk stabilization training programme, and were re-evaluated by a physiotherapist after 3–6 months. Candidates presenting with subjective training-resistant trunk symptoms after evaluation were considered eligible for inclusion. Inclusion criteria were: non smoker, age 18–55 years, BMI below 35 kg/m2, DRA greater than 30 mm on ultrasound imaging at any level, trunk instability symptoms persisting after more than 3 months of standardized trunk stability training, more than 1 year from last delivery, and no intention of further pregnancy. The presence of preoperative cosmetic issues was not considered as a symptom or as an outcome in this study. Written informed consent was obtained from all participants before inclusion. The Regional Ethics Committee, Karolinska Institutet, Stockholm, approved the study. The local ethics committee approved all procedures (Dnr. 2015/ 1753-31).
Evaluation of symptoms
The primary outcome was abdominal trunk function. Secondary outcomes were quality of life (QoL), urinary incontinence and DRA recurrence (at follow-up).
To evaluate abdominal trunk function, a standardized multimodal trunk function test was designed to cover all dysfunctions associated with symptomatic DRA: the Abdominal Trunk Function Protocol (ATFP) (Appendix S1, supporting information). The ATFP consists of a self-rating section, where the participants score physical function (Disability Rating Index (DRI)), and seven trunk function tests supervised and monitored by a physiotherapist following a strict schema. The validated DRI covers 12 non-specific activities of daily life, each one self-rated on a visual analogue scale of 0–100 mm, providing a score of 0–100 for each activity, where 0 represents no difficulty in performing the specific task and 100 indicates an inability to perform the task at all27. The seven trunk function tests have been validated separately and measure different aspects of trunk and pelvic strength, endurance and stability. They are: the back muscle strength test, the abdominal muscle strength test, the lateral core stability test (left and right side), the ventral core stability test, the active straight-leg-raising test, and the pelvic joint provocation test28,29. The trunk function tests were conducted and monitored by a physiotherapist. The ATFP evaluation was performed before and 1 year after surgery. QoL was evaluated using the self-reported Medical Outcome Survey Short Form 36 (SF-36®) (Rand Corporation, Santa Monica, California, USA)30. Urinary incontinence was evaluated using the self-reported Urogenital Distress Inventory (UDI-6) and the Incontinence Impact Questionnaire (IIQ-7) forms31. DRA recurrence was assessed by CT 1 year after surgery, and was defined as a persisting diastasis greater than 30 mm.
Surgical reconstruction technique
The surgical procedure was a standardized suture repair of the diastasis using a double-row plication with absorbable Quillâ„¢ 2/0 sutures (Angiotech, Reading, Pennsylvania, USA). Access to the linea alba depended on anatomical conditions, body figure and excess skin. The surgical procedure was categorized according to the incision made: method A used a midline incision; method B involved a low transverse incision, including limited resection of excessive
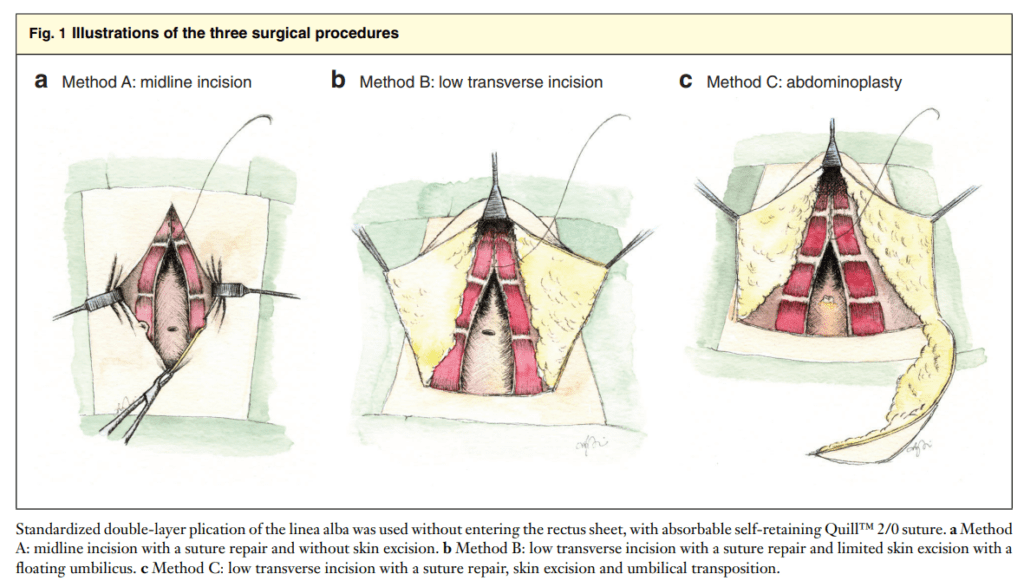
skin and a floating umbilicus; and method C employed abdominoplasty, including resection of excessive skin and umbilical transposition (Fig. 1a– c). The three methods had an identical deep muscle layer technique. The decision of which method to use was based on the anatomical circumstances and the woman’s preference (after detailed information regarding the risks associated with the different incisions).
All surgical procedures except one were performed by one of two consultant surgeons, at either the general surgical unit or the ambulatory surgical unit. All women were admitted to the ward for postoperative care. Patients operated on with methods B and C had an active 14-Fr catheter drain(s) that was removed when fluid loss was less than 50 ml/day according to local routines for ventral hernia repair. All women were instructed to wear a girdle for 12 weeks (day and night in weeks 1–8, daytime only in weeks 9–12), which has been standard (with minor adjustments) in previous studies32. Patients were also instructed to participate in a standardized rehabilitation programme developed by the physiotherapy department at the authors’ hospital (Appendix S2, supporting information), as well as daily exercise such as short walks, but to avoid heavy physical exercise during the first 12 weeks. All women were followed up clinically and with ultrasound assessment at 6–8 weeks and 1 year after surgery. All postoperative complications within 30 days were registered.
Statistical analysis
Descriptive statistics were used to characterize demography. Pairwise correlation coefficients were performed between measurements of rectus diastasis, comparing preoperative ultrasound and CT scan measurements with the width measured at surgery. For continuous variables, paired t tests and Wilcoxon signed rank tests were used to identify changes in symptoms at 1-year follow-up, and McNemar’s test was used to evaluate contingency of dichotomous variables. All tests were two-sided and considered statistically significant at a level of P ≤0.050. For the DRI, each parameter was investigated individually and the total DRI score was used for comparison purposes. SF-36® results were analysed and compared with data from 2679 women aged 15–44 years in the Swedish SF-36 Health Survey30 (Table S1, supporting information). Linear regression was used to test whether the degrees of preoperative symptoms were associated with change in those symptoms after surgery. Non-linearity was investigated by adding a quadratic term of the preoperative variable investigated in the model. Statistical analyses were performed using Stata® 12.1 (StataCorp, College Station, Texas, USA).
Results
Table 1 summarizes the preoperative demographics of the 60 women who were included in the study. Their mean age at the time of surgery was 38⋅8 (range 20⋅5–53) years. The follow-up rate was 93 per cent (56 of 60) for the DRI questionnaire, and 83 per cent (50 of 60) for the seven functional tests. There were four dropouts due to subacute orthopaedic surgery (1 patient), emigration (1), unrelated psychiatric disability (1) and declined further participation (1). A further six participants were excluded from follow-up of the functional tests owing to incomplete forms.
Surgery
Nineteen of the 60 women (32 per cent) underwent surgical method A, 31 (52 per cent) had method B, and ten (17 per cent) method C. There was at least one concomitant midline fascial defect in 45 women (75 per cent), of which six (13 per cent) were diagnosed at surgery. The correlation coefficient between the rectus diastasis measured by
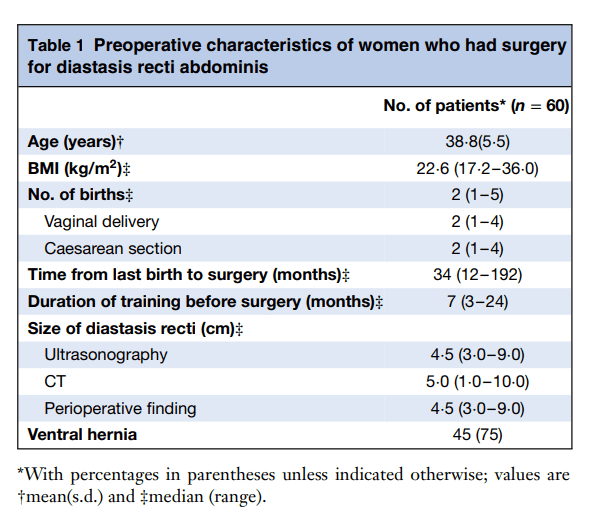
ultrasonography and the intraoperative finding was 0⋅71. The corresponding coefficient for CT was 0⋅55. In general, ultrasound imaging tended to underestimate the mean diastasis by 4 mm (P = 0⋅007) and CT overestimated by 3 mm (P = 0⋅139). The median hospital stay was 3 (range 1–8) days.
Postoperative complication and recurrence rates
At the 6–8-week follow-up, seven women had a postoperative complication. Four women (3 operated on with method B and 1 with method C) developed bleeding/haematoma that needed reoperation (Clavien–Dindo grade IIIb33,34). Two patients (operated on with method B) developed a surgical-site infection requiring antibiotic treatment (Clavien–Dindo grade II). One patient (operated on with method A) presented with spontaneous pneumothorax not requiring intervention 2 weeks after surgery (Clavien–Dindo grade I). Four patients (3 operated on with method B and 1 with method C) developed a seroma not requiring intervention, diagnosed at clinical follow-up 6–8 weeks after surgery (Clavien–Dindo grade I). Finally, four women were not satisfied with the cosmetic result due to umbilical asymmetry, of whom two had reoperation; this was not considered a complication. None of the early complications had led to long-term sequelae at the 1-year follow-up. Complications according to the Clavien–Dindo classification33,34 were in summary: grade I, five of 60 (8 per cent); grade II, two of 60 (3 per cent); grade IIIb, four of 60 (7 per cent). No recurrences were observed at 6–8 weeks or at 1-year follow-up.
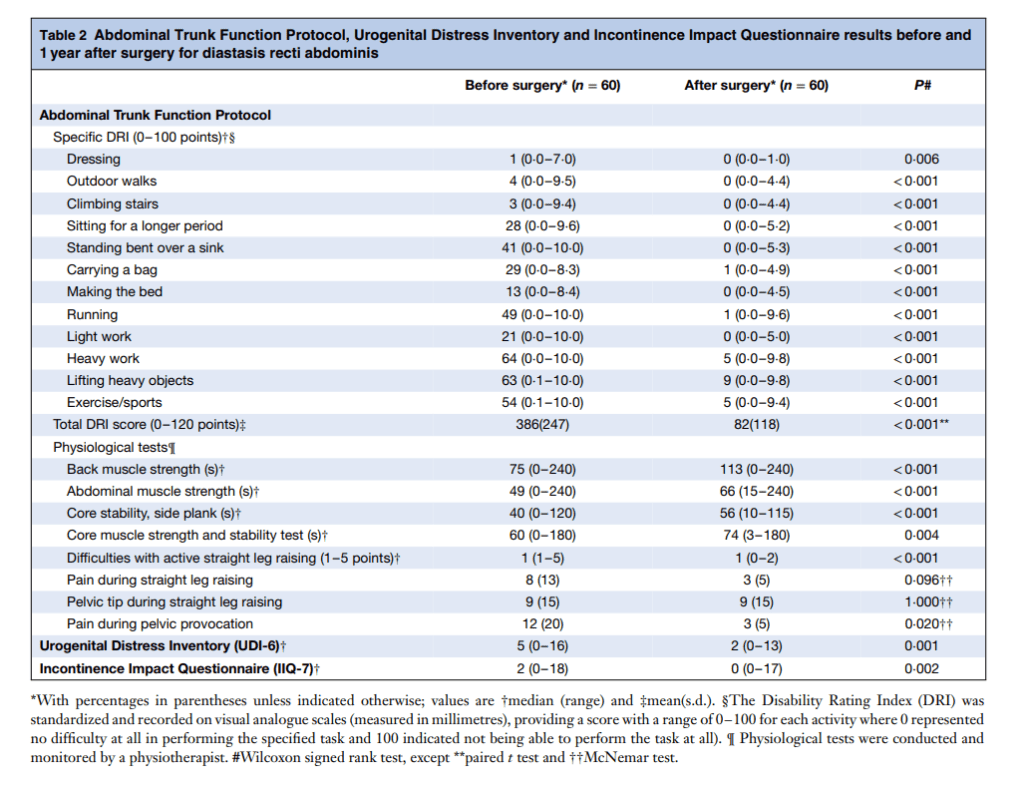
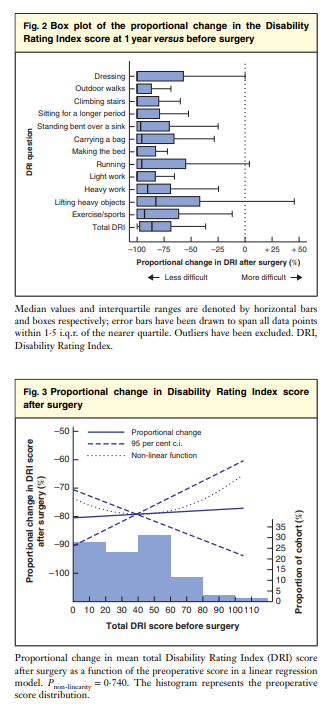
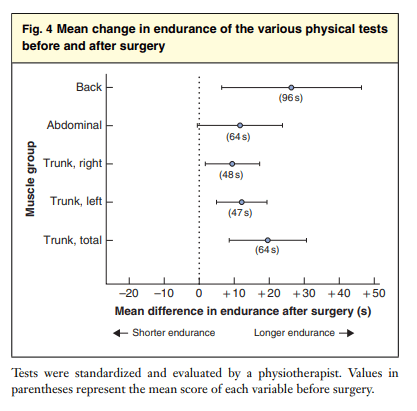
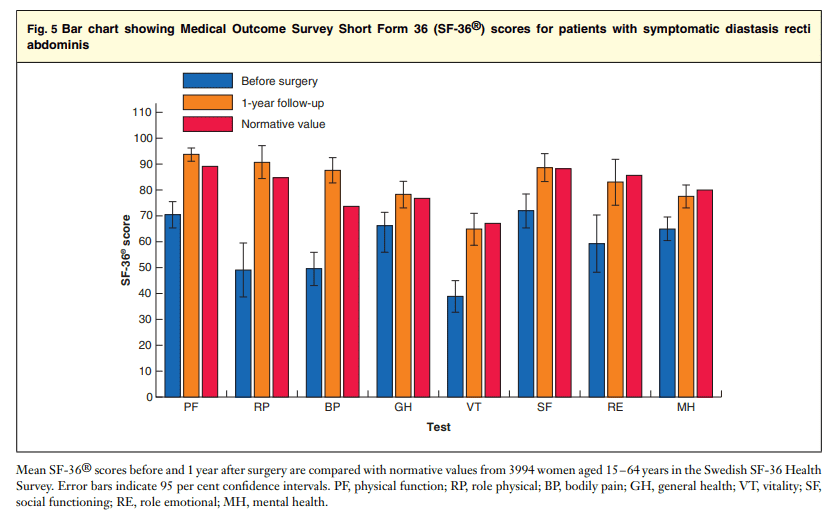
Abdominal Trunk Function Protocol Table 2 summarizes the ATFP findings before surgery and at 1-year follow-up. Regarding the DRI, 98 per cent of women (55 of 56) reported fewer problems after surgery, and the total scores were, on average, 79â‹…1 (95 per cent c.i. 73â‹…1 to 85â‹…1) per cent lower at follow-up than before surgery. One patient reported a higher score after surgery (total DRI 98 before surgery versus 105 after surgery). Median scores and proportional change after surgery for each specific question are displayed in Fig. 2. The preoperative score was not associated with proportional change in DRI at follow-up (P =0â‹…804) (Fig. 3). When evaluated by a physiotherapist, a majority of patients (38 of 50, 76 per cent) had significantly better performance and stamina at follow-up than before surgery. There was no significant change in pain and pelvic tip during straight leg raising. Although a significant proportion of the women performed better in the postoperative tests, the mean abdominal strength did not appear to have improved at 1-year follow-up (Fig. 4).
Quality of life
Mean SF-36® subscale scores, comparing results before and after surgery, and with expected ratings in a normative Swedish female population, are shown in Fig. 5. Before surgery, the women generally had a lower QoL than the normative Swedish female population in all SF-36® subscales (P <0.003). After surgery, their QoL improved significantly, with scores similar to those of the normative Swedish female population in all subscales, and even higher in terms of bodily pain (P <0.001).
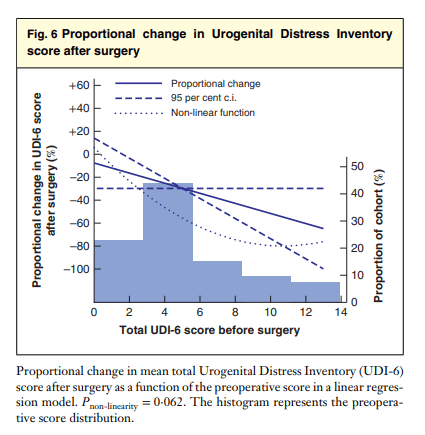
Urinary incontinence
Table 2 summarizes urinary incontinence before surgery and at 1-year follow-up. A general decrease in incontinence symptoms was observed after surgery, with 28 of the 60 women (47 per cent) reporting a lower score in the UDI-6 after surgery, and eight (13 per cent) reporting a higher score. The mean reduction in score after surgery was 34.4 (95 per cent c.i. 16.4 to 52.3) per cent. There appeared to be an inverse linear relationship between scores before and after surgery, with each point scored before surgery related to a 0.39-point decrease in UDI-6 after surgery. Although no formal evidence of non-linearity was observed (P = 0â‹…062), no relief of symptoms was observed after surgery when 2 or fewer points were scored before surgery. Otherwise, the proportional decrease in UDI-6 score remained between 40 and 80 per cent (Fig. 6).
For the IIQ-7, 22 of the 60 women (37 per cent) had fewer symptoms and five (8 per cent) experienced more symptoms.
Discussion
DRA is a potentially debilitating condition in postpartum women that correlates with trunk instability, urinary incontinence and impaired QoL. In this study, a significant improvement in self-reported disability and physical performance, higher QoL and reduced urinary incontinence was observed in the majority of women after surgical treatment of DRA. A novel multimodal protocol to evaluate abdominal trunk function was also introduced.
All women reported a better QoL (SF-36® findings) after surgery, reaching levels similar to those in a normative Swedish female population, regardless of performed surgical method. This indicates that the selection process was successful in distinguishing between physical and cosmetic reasons for surgery. The ATFP focused on functional disability that was resistant to training, thereby selecting patients likely to benefit from surgery. The fact that proportional improvements in DRI and physical tests were similar for all patients, regardless of preoperative scores, implies that surgical reconstruction leads to improvement in function in all postpartum women with DRA. With respect to the postoperative rehabilitation programme, it is not likely that rehabilitation with a lower load than the preoperative training would have had any significant impact on the improvement.
It is suggested that patients with DRA not causing dysfunction (DRA less than 30 mm, midline hernia or cosmetic issues) should first and foremost receive conservative management with weight control, limited hernia repair or purely aesthetic surgery. Evidence in the literature supporting physical training for symptomatic DRA18 –21 is inconclusive. The main purpose of physical training is possibly
to restore function, and not necessarily to reduce the diastasis. If physical training proves to be unsuccessful, surgical reconstruction may be the next step in the treatment algorithm.
The improvement in urinary incontinence symptoms observed in this study is in line with previous studies26, and may indicate a correlation between abdominal trunk instability and pelvic floor dysfunction. Higher preoperative UDI-6 scores resulted in greater improvements in urinary incontinence symptoms after surgery, suggesting that patients with severe symptoms benefit more from surgical reconstruction than those with mild symptoms – an important factor when selecting patients for surgery.
All three surgical techniques used in this study provided similar results regarding outcome and recurrence. None of the women had signs of recurrence 1 year after surgery, and the complication rate was similar to that following other medium-sized surgery such as open ventral hernia repair. There were no differences in QoL outcomes between the three surgical methods, indicating that cosmetic improvement alone was unlikely to be the reason for the improvement in QoL.
The high incidence of perioperative ventral hernia in the study sample could indicate that these hernias contributed to the symptoms; however, the presenting symptoms are not usually associated with a ventral hernia and it is unlikely that the concurrent hernia repair alone could explain the results.
This study has limitations. It lacked a conservatively managed control group, which makes any far reaching conclusion difficult as some beneficial effects could have been a placebo effect or simply due to the passing of time, although comparison of preoperative and postoperative results allows within-person changes to be measured. The inclusion criteria were restricted to patients with symptomatic persistent DRA, and these results are thus not applicable to all patients with postpartum DRA.
During pregnancy, women are at risk of developing persistent symptomatic DRA that may have a detrimental effect on their physical function and QoL. This study has demonstrated that surgical reconstruction of DRA in postpartum women with symptoms resistant to training results in significant improvements in abdominal trunk function, urinary incontinence and QoL for a majority of patients. Surgical reconstruction of DRA is a valid alternative for patients presenting with symptomatic DRA, where adequate physical training has proven unsuccessful.
Acknowledgements
The authors acknowledge physiotherapist L. Nordstrand for thorough functional examinations, and L. Bai for her illustrations of the surgical procedures employed.
This work was funded by grants from Stockholm County Council and the Swedish Society of Medicine.
Disclosure: The authors declare no conflict of interest.
References
1. Boissonnault JS, Blaschak MJ. Incidence of diastasis recti abdominis during the childbearing year. Phys Ther 1988; 68:1082–1086.
2. Noble E. Essential Exercises for the Childbearing Year (3rd edn). Houghton Mifflin: Boston, 1988.
3. Beer GM, Schuster A, Seifert B, Manestar M, Mihic-Probst D, Weber SA. The normal width of the linea alba in nulliparous women. Clin Anat 2009; 22: 706–711.
4. Rath AM, Attali P, Dumas JL, Goldlust D, Zhang J, Chevrel JP. The abdominal linea alba: an anatomo-radiologic and biomechanical study. Surg Radiol Anat 1996; 18: 281–288.
5. Emanuelsson P, Dahlstrand U, Strömsten U, Gunnarsson U, Strigård K, Stark B. Analysis of the abdominal musculo-aponeurotic anatomy in rectus diastasis: comparison of CT scanning and preoperative clinical assessment with direct measurement intraoperatively. Hernia 2014; 18: 465–471.
6. Akram J, Matzen SH. Rectus abdominis diastasis. J Plast Surg Hand Surg 2014; 48: 163–169.
7. Sperstad JB, Tennfjord MK, Hilde G, Ellström-Engh M, Bø K. Diastasis recti abdominis during pregnancy and 12 months after childbirth: prevalence, risk factors and report of lumbopelvic pain. Br J Sports Med 2016; 50: 1092–1096.
8. Fernandes da Mota PG, Pascoal AG, Carita AI, Bø K. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther 2015; 20: 200–205.
9. Gitta S, Magyar Z, Tardi P, Füge I, Járomi M, Ãcs P et al. Prevalence, potential risk factors and sequelae of diastasis recti abdominis. Orv Hetil 2017; 158: 454–460.
10. Candido G, Lo T, Janssen PA. Risk factors for diastasis of the recti abdominis. Journal of the Association of Chartered Physiotherapists in Women’s Health 2005; 97: 49–54.
11. Hills NF, Graham RB, McLean L. Comparison of trunk muscle function between women with and without diastasis recti abdominis at 1 year postpartum. Phys Ther 2018; 98: 891–901.
12. Parker M, Millar L, Dugan S. Diastasis rectus abdominis and lumbo-pelvic pain and dysfunction – are they related? J Womens Health Phys Therap 2009; 33: 15–22.
13. Spitznagle TM, Leong FC, Van Dillen LR. Prevalence of diastasis recti abdominis in a urogynecological patient population. Int Urogynecol J Pelvic Floor Dysfunct 2007; 18: 321–328.
14. Doubkova L, Andel R, Palascakova-Springrova I, Kolar P, Kriz J, Kobesova A. Diastasis of rectus abdominis muscles in low back pain patients. J Back Musculoskelet Rehabil 2018; 31: 107–112.
15. Gutke A, Ostgaard HC, Oberg B. Association between muscle function and low back pain in relation to pregnancy. J Rehabil Med 2008; 40: 304–311.
16. Ostgaard HC, Zetherström G, Roos-Hansson E. Back pain in relation to pregnancy: a 6-year follow-up. Spine (Phila Pa 1976) 1997; 22: 2945–2950.
17. To WW, Wong MW. Factors associated with back pain symptoms in pregnancy and the persistence of pain 2 years after pregnancy. Acta Obstet Gynecol Scand 2003; 82: 1086–1091.
18. Benjamin DR, van de Water AT, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy 2014; 100: 1–8.
19. Mesquita LA, Machado AV, Andrade AV. Physiotherapy for reduction of diastasis of the recti abdominis muscles in the postpartum period. Rev Bras Ginecol Obstet 1999; 21: 267–272.
20. Mommers EHH, Ponten JEH, Al Omar AK, de Vries Reilingh TS, Bouvy ND, Nienhuijs SW. The general surgeon’s perspective of rectus diastasis. A systematic review of treatment options. Surg Endosc 2017; 31: 4934–4949.
21. Lee D, Hodges PW. Behavior of the linea alba during a curl-up task in diastasis rectus abdominis: an observational study. J Orthop Sports Phys Ther 2016; 46: 580–589.
22. Toranto IR. The relief of low back pain with the WARP abdominoplasty: a preliminary report. Plast Reconstr Surg 1990; 85: 545–555.
23. Oneal RM, Mulka JP, Shapiro P, Hing D, Cavaliere C. Wide abdominal rectus plication abdominoplasty for the treatment of chronic intractable low back pain. Plast Reconstr Surg 2011; 127: 225–231.
24. Emanuelsson P, Gunnarsson U, Dahlstrand U, Strigård K, Stark B. Operative correction of abdominal rectus diastasis (ARD) reduces pain and improves abdominal wall muscle strength: a randomized, prospective trial comparing retromuscular mesh repair to double-row, self-retaining sutures. Surgery 2016; 160: 1367–1375.
25. Nahas FX, Augusto SM, Ghelfond C. Should diastasis recti be corrected? Aesthetic Plast Surg 1997; 21: 285–289.
26. Taylor DA, Merten SL, Sandercoe GD, Gahankari D, Ingram SB, Moncrieff NJ et al. Abdominoplasty improves low back pain and urinary incontinence. Plast Reconstr Surg 2018; 141: 637–645.
27. Salén BA, Spangfort EV, Nygren AL, Nordemar R. The Disability Rating Index: an instrument for the assessment of disability in clinical settings. J Clin Epidemiol 1994; 47: 1423–1435.
28. Biering-Sørensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine (Phila Pa 1976) 1984; 9: 106–119.
29. Laslett M, Young SB, Aprill CN, McDonald B. Diagnosing painful sacroiliac joints: a validity study of a McKenzie evaluation and sacroiliac provocation tests. Aust J Physiother 2003; 49: 89–97.
30. Sullivan M, Karlsson J, Ware JE Jr. The Swedish SF-36 Health Survey – I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med 1995; 41: 1349–1358.
31. Franzén K, Johansson JE, Karlsson J, Nilsson K. Validation of the Swedish version of the incontinence impact questionnaire and the urogenital distress inventory. Acta Obstet Gynecol Scand 2013; 92: 555–561.
32. Emanuelsson P. Alternatives in the Treatment of Abdominal Rectus Muscle Diastasis: an Evaluation; 2014. https:// openarchive.ki.se/xmlui/handle/10616/42245 [accessed 15 January 2019].
33. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD et al. The Clavien–Dindo classification of surgical complications: five-year experience. Ann Surg 2009; 250: 187–196.
34. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004; 240: 205–213.